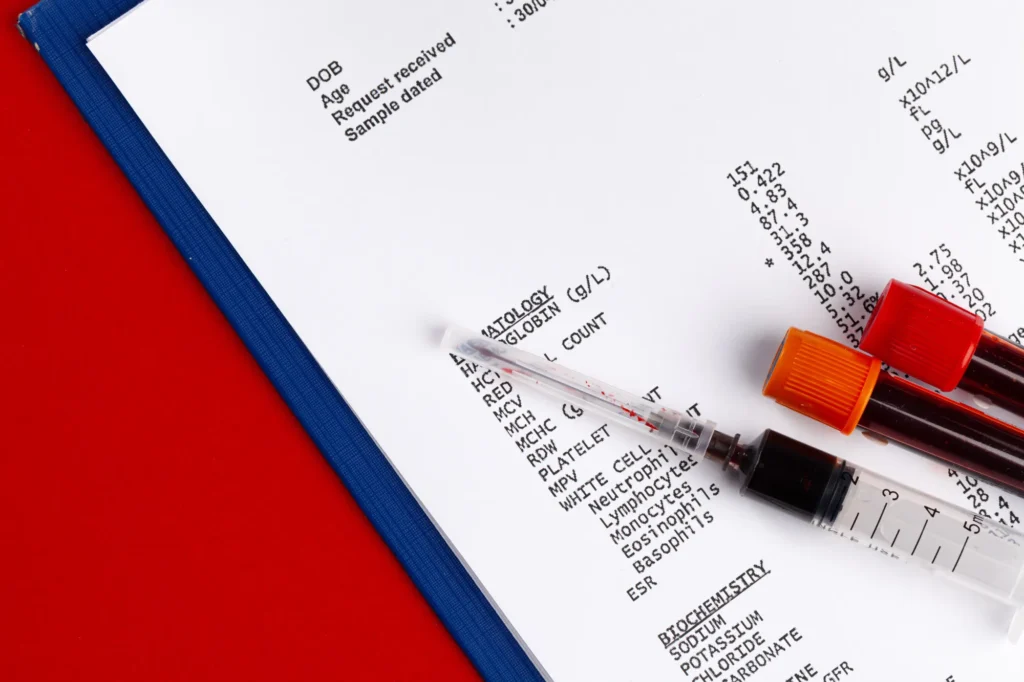
For millions of women worldwide, routine blood testing is a fundamental aspect of healthcare—used to track hormone levels, assess metabolic function, and detect underlying health conditions. However, few realize that the timing of these tests in relation to their menstrual cycle can significantly influence the results. Variations in estrogen, progesterone, and other hormones affect biomarkers such as cholesterol, inflammation markers, and iron levels, leading to potential misinterpretations if cycle phase is not accounted for.
Understanding these fluctuations is critical for accurate diagnostics. Women who test at different points in their cycle may see inconsistent results, making it difficult to monitor long-term health trends effectively. To ensure reliability, experts recommend that women schedule blood tests consistently within the same phase of their cycle.
This article explores how menstrual cycle phases impact blood test biomarkers, offering insights into optimal test timing and the physiological mechanisms driving these variations.
In This Article
How the Menstrual Cycle Affects Blood Test Results
The menstrual cycle is divided into four distinct phases:
- Menstrual Phase (Days 1–5): Hormone levels are at their lowest as the uterine lining sheds, leading to potential decreases in iron and hemoglobin.
- Follicular Phase (Days 1–14): Estrogen levels gradually rise, influencing lipid profiles and inflammatory markers.
- Ovulation Phase (Around Day 14): A surge in luteinizing hormone (LH) and peak estrogen levels occur, impacting various metabolic processes.
- Luteal Phase (Days 15–28): Progesterone dominates, affecting cholesterol, glucose metabolism, and inflammation.
These hormonal fluctuations create measurable variations in blood biomarkers, which must be considered when interpreting test results.
Table 1: Overview of Hormonal Changes Across the Menstrual Cycle
| Menstrual Phase | Estrogen | Progesterone | Key Biomarker Changes |
|---|---|---|---|
| Menstrual (Days 1–5) | Low | Low | Decreased iron, lower hemoglobin |
| Follicular (Days 1–14) | Increasing | Low | Stable lipid profile, reduced inflammation |
| Ovulation (~Day 14) | Peak | Low | Increased LH, estrogen surge |
| Luteal (Days 15–28) | High | High | Increased cholesterol, higher inflammatory markers |
Biomarkers Affected by Menstrual Cycle Phases
1. Iron and Hemoglobin
Menstrual bleeding naturally reduces iron levels, particularly in women with heavy periods. Studies indicate that iron biomarkers, including ferritin, hemoglobin, and transferrin saturation, are lowest during menstruation and highest in the luteal phase. This means women who test for anemia during their period may receive an artificially low result.
Key Insight: Women concerned about iron deficiency should schedule tests in the mid-luteal phase for more stable readings.
2. Lipid Profile and Cholesterol
Cholesterol levels fluctuate throughout the menstrual cycle, with total cholesterol and LDL (“bad” cholesterol) tending to rise in the luteal phase due to progesterone dominance. A study published in The Journal of Clinical Endocrinology & Metabolism found that HDL (“good” cholesterol) is typically highest during the follicular phase.
Key Insight: For consistent cholesterol monitoring, testing should be done at the same cycle phase each time, preferably during the follicular phase when levels are most stable.
3. Inflammation Markers (hs-CRP)
High-sensitivity C-reactive protein (hs-CRP), an indicator of inflammation, shows cyclical variation. Research suggests that hs-CRP levels peak during menstruation, decline throughout the follicular phase, and rise again in the luteal phase.
Key Insight: If testing for inflammation or autoimmune conditions, women should avoid scheduling tests during menstruation to prevent misleadingly high readings.
4. Hormones (Estradiol, Progesterone, LH, FSH)
Hormone tests must be timed carefully, as levels vary dramatically across the cycle.
- Estradiol is lowest during menstruation, peaks just before ovulation, and remains elevated in the luteal phase.
- Progesterone remains low until ovulation and reaches its highest point in the luteal phase.
- LH and FSH spike during ovulation but are otherwise relatively stable.
Key Insight: Women tracking fertility or hormone imbalances should follow physician guidelines on optimal test timing based on their cycle.
5. Vitamin D Levels
Surprisingly, vitamin D levels fluctuate across the menstrual cycle, with some research indicating higher levels during menstruation. One study in Endocrine Connections suggested that this variation may be linked to estrogen’s role in vitamin D metabolism.
Key Insight: If testing for vitamin D deficiency, results should be interpreted in the context of menstrual cycle phase.
Best Practices for Timing Blood Tests
To improve test accuracy, consider these best practices:
- Consistency is Key: Schedule blood tests at the same cycle phase each time for reliable comparisons.
- Track Your Cycle: Use an app or journal to monitor menstrual phases and inform testing decisions.
- Consult Your Doctor: If testing hormone levels, confirm the optimal day for sample collection.
- Avoid Menstruation for Iron Tests: Low readings during menstruation may not reflect true iron status.
- Choose the Follicular Phase for Lipid Tests: Cholesterol levels are most stable in this phase.
Table 2: Recommended Blood Test Timing Based on Menstrual Phase
| Blood Test | Best Time for Testing | Reason |
|---|---|---|
| Iron Panel | Mid-luteal phase | Avoids low levels from menstrual bleeding |
| Lipid Profile | Early follicular phase | Provides the most stable readings |
| hs-CRP (Inflammation Marker) | Mid-follicular phase | Avoids inflammatory peaks during menstruation |
| Hormone Panel (Estrogen, Progesterone, LH, FSH) | Depends on test | Timing varies based on cycle phase |
| Vitamin D | Any phase (but consistent) | Levels fluctuate slightly across cycle |
Conclusion
Blood test results can vary significantly based on menstrual cycle phase, making it essential for women to time their tests consistently. Understanding these variations helps prevent misinterpretations and ensures reliable tracking of health metrics over time.
By aligning blood tests with specific cycle phases, women and healthcare providers can make more accurate diagnoses and treatment decisions. Whether monitoring cholesterol, inflammation, or hormone levels, strategic scheduling enhances the precision of test results—empowering women to take control of their health with data they can trust.
References
- Chiazze L Jr, Brayer FT, Macisco JJ Jr, Parker MP, Duffy BJ. The length and variability of the human menstrual cycle. JAMA. 1968;203(6):377-380.
- Lenton EA, Landgren BM, Sexton L, Harper R. Normal variation in the length of the luteal phase of the menstrual cycle: identification of the short luteal phase. Br J Obstet Gynaecol. 1984;91(7):685-689.
- Mumford SL, Schisterman EF, Siega-Riz AM, Gaskins AJ, Steiner AZ, Daniels JL, et al. A longitudinal study of serum lipoproteins in relation to endogenous reproductive hormones during the menstrual cycle: findings from the BioCycle Study. J Clin Endocrinol Metab. 2010;95(9):E80-E85.
- Roney JR, Simmons ZL. Elevated psychological stress predicts reduced estradiol concentrations in young women. Am J Hum Biol. 2015;27(4):501-507.
- Gaskins AJ, Mumford SL, Zhang C, Wactawski-Wende J, Hovey KM, Whitcomb BW, et al. Effect of daily fiber intake on reproductive function: the BioCycle Study. Am J Clin Nutr. 2009;90(4):1061-1069.





0 Comments