Adrenal masses are frequently discovered incidentally during imaging for unrelated conditions, a phenomenon increasingly common in modern clinical practice. Among these adrenal incidentalomas, adrenal pseudocysts represent a rare yet clinically significant subtype. Although typically benign, adrenal pseudocysts can pose a diagnostic dilemma due to their non-specific clinical presentation and radiological similarity to malignant or infectious lesions. Their rarity often leads to confusion with other adrenal and retroperitoneal pathologies, sometimes resulting in delayed or inappropriate treatment.
Understanding adrenal pseudocysts is essential for healthcare professionals involved in diagnosing or managing adrenal abnormalities. While their benign nature may suggest a conservative approach, the diagnostic ambiguity necessitates a careful and sometimes aggressive workup to rule out malignancy or functional endocrine tumors. This article explores the etiology, clinical presentation, diagnostic challenges, and management strategies associated with adrenal pseudocysts, reinforcing the central thesis: adrenal pseudocysts are rare but can mimic other conditions, making accurate diagnosis essential for appropriate management.
In This Article
What Is an Adrenal Pseudocyst?
Adrenal pseudocysts are encapsulated, cystic lesions of the adrenal gland that lack an epithelial or endothelial lining—a key histological feature distinguishing them from true cysts. Instead, they are surrounded by fibrous tissue and often contain hemorrhagic, serous, or necrotic debris. First described in the mid-20th century, adrenal pseudocysts account for less than 5% of all adrenal cystic lesions and often arise as a result of prior hemorrhage, trauma, or degenerative changes within the adrenal parenchyma.
They are typically non-functional, meaning they do not produce excess adrenal hormones, though rare exceptions have been documented. Their etiology remains somewhat obscure, but several contributing mechanisms have been proposed, including:
- Previous adrenal hemorrhage
- Degeneration of a neoplasm (e.g., a necrotic adrenal cortical carcinoma)
- Vascular abnormalities
- Trauma or infection
Epidemiology and Classification of Adrenal Cystic Lesions
Although adrenal pseudocysts are rare, they form part of a broader classification system for adrenal cysts. These lesions are generally divided into four main types:
| Type | Defining Feature | Prevalence |
|---|---|---|
| Endothelial cysts | Lined by endothelium (lymphangiomatous or angiomatous) | ~45% |
| Pseudocysts | No lining, fibrous wall, often hemorrhagic | ~39% |
| Epithelial cysts | Lined by epithelial cells | ~9% |
| Parasitic cysts | Often caused by Echinococcus species | ~7% |
(Source: Foster, D. W., & Endocrinology Texts, 2022)
Pseudocysts are the second most common type and are predominantly unilateral, with a slight female predominance. They can range in size from a few centimeters to over 20 cm in diameter, with some reported to cause mass effect or retroperitoneal hemorrhage due to rupture.
Clinical Presentation: Often Silent, Sometimes Striking
Most adrenal pseudocysts are asymptomatic and discovered incidentally. However, symptomatic presentations can occur and often relate to the lesion’s size, anatomical location, or complications such as hemorrhage or infection. Symptoms, when present, may include:
- Abdominal or flank pain
- Nausea and vomiting
- Palpable mass
- Hypertension (rare)
- Symptoms of hemorrhage (e.g., hypotension, anemia, retroperitoneal pain)
Rarely, adrenal pseudocysts may coexist with hormonally active tumors, producing features of Cushing’s syndrome or pheochromocytoma, further complicating diagnosis.
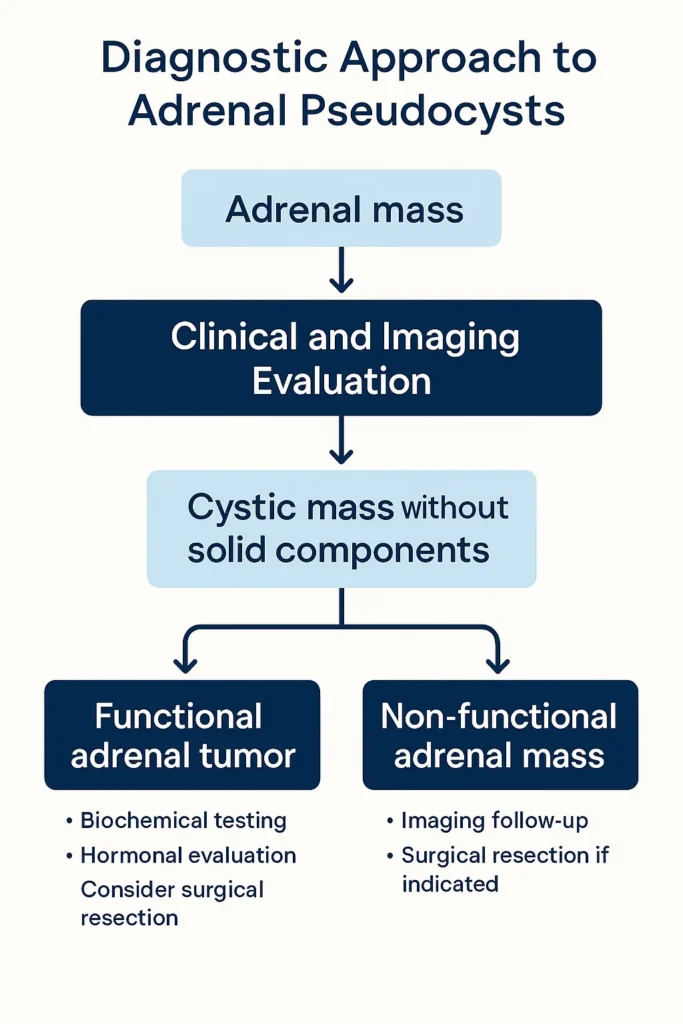
Diagnostic Challenges: Differentiating Pseudocysts from Malignancy
One of the key clinical concerns with adrenal pseudocysts is their potential to mimic more serious pathology, particularly adrenal cortical carcinoma (ACC), cystic pheochromocytoma, or metastasis. Radiologically, the absence of characteristic features can make it difficult to distinguish pseudocysts from malignant masses. Thus, diagnostic imaging and biochemical evaluation become pivotal.
Imaging Modalities and Their Limitations
- Ultrasound (US):
- May reveal an anechoic or mixed echogenic mass.
- Limited utility due to overlying bowel gas and retroperitoneal depth.
- Computed Tomography (CT):
- Typically shows a well-encapsulated cystic mass.
- Hemorrhagic contents may appear hyperdense.
- No solid enhancing components suggest benignity but do not exclude malignancy.
- Magnetic Resonance Imaging (MRI):
- Superior at characterizing fluid content and hemorrhage.
- High signal intensity on T1-weighted images indicates blood products.
- Low signal on T2-weighted images may suggest chronic hemorrhage or fibrotic content.
- Positron Emission Tomography (PET):
- Useful if malignancy is strongly suspected.
- Lack of uptake supports benignity but isn’t definitive.
Biochemical Testing
Routine endocrine workup includes:
- Plasma metanephrines or 24-hour urinary catecholamines (rule out pheochromocytoma)
- Dexamethasone suppression test (rule out cortisol-producing tumor)
- Serum aldosterone and renin (for aldosterone-producing lesions)
Most adrenal pseudocysts are hormonally inactive, but thorough testing is crucial to avoid missing a functional lesion.
Histopathology: The Gold Standard for Diagnosis
Definitive diagnosis of an adrenal pseudocyst is histological. Key features include:
- Absence of epithelial lining
- Thick fibrous capsule
- Intra-cystic hemorrhage or necrosis
- Absence of neoplastic cells
Pathologic examination is typically performed post-surgical resection, especially when imaging and clinical findings are inconclusive.
Management Strategies: When to Observe and When to Excise
Management of adrenal pseudocysts depends on multiple factors, including:
- Size
- Symptomatology
- Imaging features
- Hormonal activity
- Malignancy suspicion
Observation
Small (<4 cm), asymptomatic, and non-functioning cysts with benign imaging features may be observed with periodic imaging. Repeat CT or MRI at 6-12 month intervals is often recommended.
Surgical Resection
Surgical intervention is indicated when:
- Lesion >5-6 cm due to higher risk of malignancy
- Symptoms are present
- Hormonal activity is detected
- Imaging features are ambiguous or concerning
- Rapid growth is documented on serial imaging
Laparoscopic adrenalectomy is the preferred approach for most cases, offering lower morbidity than open surgery. However, very large or invasive lesions may require an open approach.
Prognosis and Follow-Up
The prognosis for adrenal pseudocysts is excellent when malignancy is excluded. Recurrence is rare after complete resection. Follow-up typically involves:
- Imaging at 6-12 months post-resection
- Endocrine evaluation if initial tests were abnormal
- Periodic imaging for unresected lesions
Case Studies Highlighting Diagnostic Complexity
Case 1: Misdiagnosed Adrenal Carcinoma
A 45-year-old woman presented with left upper quadrant pain. CT showed a 7 cm complex cystic adrenal mass with calcifications. PET scan revealed low uptake. Surgical resection revealed a hemorrhagic adrenal pseudocyst—benign despite radiological concern.
Case 2: Functional Tumor Overlooked
A 38-year-old man with hypertension and a 4.5 cm adrenal cyst was diagnosed with a pseudocyst on imaging. Further hormonal tests revealed elevated metanephrines. The final diagnosis was cystic pheochromocytoma. This case highlights the importance of not skipping hormonal evaluation.
Practical Takeaways for Clinicians and Patients
- Always perform a full hormonal workup, even when the lesion appears benign.
- Lesions >5 cm should be approached with caution and often warrant resection.
- Imaging alone cannot definitively distinguish pseudocysts from malignancies.
- Histological confirmation remains the gold standard.
- Patient education is critical: most adrenal incidentalomas are benign, but proper workup is non-negotiable.
Conclusion: The Imperative of Precision in Diagnosing Adrenal Pseudocysts
Adrenal pseudocysts, though rare and typically benign, exemplify the diagnostic complexity that often accompanies adrenal lesions. Their ability to mimic malignant or functional adrenal tumors underscores the necessity for a comprehensive, multidisciplinary approach to diagnosis and management. Clinicians must combine imaging, biochemical testing, and, when necessary, surgical exploration to arrive at an accurate diagnosis. In a field where overlooking malignancy or a functional tumor can carry serious consequences, careful evaluation is more than prudent—it is essential.
References
- Foster, D. W., & Jameson, J. L. (2022). Endocrinology: Adult and Pediatric. Elsevier Health Sciences.
- Mayo Clinic Proceedings. (2021). “Adrenal Cystic Lesions: Diagnosis and Management Guidelines.”
- NIH Imaging Database. (2023). “CT and MRI Findings in Adrenal Cystic Tumors.”
- Lee, J. M., et al. (2020). “Histopathologic Differentiation of Adrenal Pseudocyst and Cystic Neoplasm.” Journal of Surgical Pathology. https://journals.lww.com/pathologycasereviews/abstract/2005/09000/adrenal_pseudocysts.7.aspx
- American Association of Clinical Endocrinologists (AACE). (2023). Adrenal Incidentaloma Clinical Practice Guidelines.
- McCauley, L. R., et al. (2021). “Management of Rare Adrenal Lesions.” Journal of Clinical Imaging Science.



0 Comments