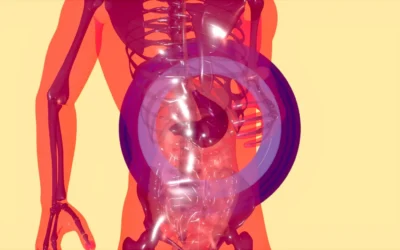
The adrenal glands, though small in size, play a pivotal role in regulating essential hormonal functions such as metabolism, blood pressure, and stress response. Damage to these glands can have far-reaching consequences, particularly when bleeding (hemorrhage) occurs within the adrenal tissue. Adrenal hemorrhage is a rare but potentially life-threatening condition, often presenting diagnostic and therapeutic challenges due to its nonspecific symptoms and varied etiologies. Over time, chronic or resolved hemorrhage can result in calcification of adrenal tissue, a radiologic finding that may indicate prior trauma, underlying disease, or infection.
Understanding adrenal hemorrhage calcification is crucial for clinicians and radiologists, as it may serve as a clue to previously unrecognized adrenal pathology or systemic illness. Moreover, the presence of adrenal calcification can influence the diagnostic approach, guide treatment decisions, and help anticipate potential endocrine complications, including adrenal insufficiency.
This article provides a comprehensive overview of adrenal hemorrhage, its causes, progression to calcification, clinical implications, diagnostic strategies, and current treatment options, all grounded in recent medical literature and clinical best practices.
In This Article
Understanding Adrenal Hemorrhage: A Clinical Overview
Adrenal hemorrhage refers to bleeding into the adrenal glands. It can be unilateral or bilateral, with the latter posing a significantly higher risk of adrenal crisis—a potentially fatal condition due to acute adrenal insufficiency.
Etiology and Risk Factors
Adrenal hemorrhage can result from various triggers, categorized as traumatic or non-traumatic:
- Traumatic causes: blunt abdominal trauma, surgery, or invasive procedures.
- Non-traumatic causes:
- Sepsis (especially meningococcemia)
- Anticoagulant therapy
- Coagulopathies
- Adrenal vein thrombosis
- Autoimmune conditions
- Pregnancy-related conditions (e.g., preeclampsia, HELLP syndrome)
- Tumors (e.g., pheochromocytoma, metastases)
A growing body of research suggests that adrenal glands are particularly susceptible to hemorrhage due to their rich arterial supply and single venous drainage. During times of physiological stress, such as sepsis or trauma, increased vascular pressure can rupture adrenal capillaries, resulting in hemorrhage.
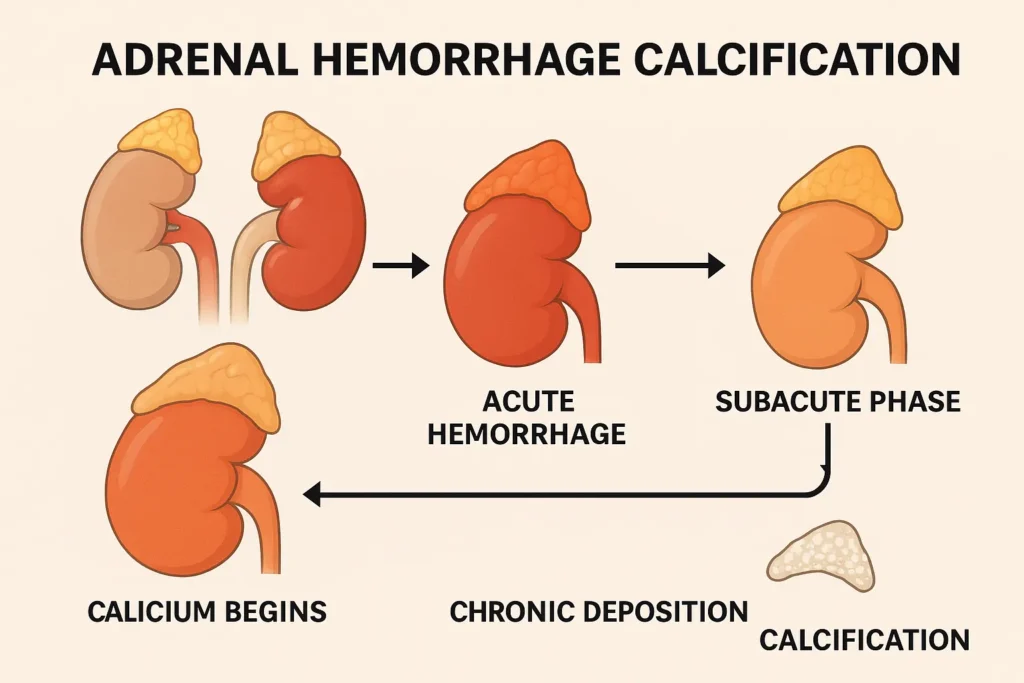
From Hemorrhage to Calcification: The Pathophysiology
When adrenal hemorrhage occurs, the body initiates a series of responses to contain and repair the damage. Over time, if the hemorrhagic insult is not fatal or does not result in total glandular necrosis, the residual hematoma may undergo organization and mineralization—a process that leads to calcification.
Stages of Progression
| Stage of Progression | Pathological Feature | Imaging Appearance |
|---|---|---|
| Acute Hemorrhage | Active bleeding, gland enlargement | Hyperdense mass on CT |
| Subacute Phase | Clot resorption, fibrosis begins | Heterogeneous mass, intermediate density |
| Chronic Phase | Hematoma resolved, calcium deposition | Dense calcification on CT |
Calcification typically takes weeks to months to develop and is often incidentally found on imaging studies performed for unrelated reasons. In neonates, this process may occur more rapidly due to their fragile vasculature and common birth-related stresses.
Clinical Presentation and Diagnostic Clues
Adrenal hemorrhage is a diagnostic challenge due to its varied and often silent clinical presentation. Acute hemorrhage may present with:
- Sudden-onset flank or abdominal pain
- Hypotension
- Fever
- Electrolyte imbalances
- Signs of adrenal insufficiency (if bilateral)
In contrast, calcified adrenal hemorrhage is usually asymptomatic, discovered during imaging for other concerns. However, its presence should prompt clinicians to investigate for previous adrenal injury or underlying systemic disorders.
Diagnostic Imaging
Modern imaging plays a central role in identifying adrenal hemorrhage and subsequent calcification.
| Imaging Modality | Utility in Adrenal Hemorrhage |
|---|---|
| CT Scan | Best for detecting acute bleeding and calcifications |
| MRI | Useful for characterizing adrenal masses and distinguishing hemorrhage from tumors |
| Ultrasound | Often used in neonates; limited in adults |
In acute hemorrhage, CT may show a hyperdense adrenal mass without contrast enhancement. In chronic stages, dense, often bilateral calcifications with or without volume loss of the adrenal glands can be seen.
Neonatal vs. Adult Adrenal Hemorrhage: A Key Distinction
Adrenal hemorrhage is relatively common in neonates, occurring in up to 1.8 per 1,000 live births, often related to birth trauma, hypoxia, or difficult delivery. In these cases, adrenal calcification can be detected within weeks after birth.
In adults, adrenal hemorrhage is rarer and usually secondary to severe systemic stress or coagulopathies. Adult adrenal calcification typically indicates a resolved past event and is more likely associated with chronic illness or malignancy.
| Feature | Neonatal Hemorrhage | Adult Hemorrhage |
|---|---|---|
| Common Causes | Birth trauma, hypoxia | Sepsis, anticoagulation |
| Frequency | Relatively common | Rare |
| Progression to Calcification | Weeks | Months |
| Clinical Concern | Adrenal function, tumor mimic | Adrenal insufficiency, neoplasm |
Adrenal Calcification and Adrenal Insufficiency
One of the key clinical implications of adrenal hemorrhage calcification is the potential for primary adrenal insufficiency. Bilateral adrenal hemorrhage can destroy a large portion of adrenal tissue, leading to decreased cortisol and aldosterone production.
Symptoms of adrenal insufficiency include:
- Fatigue
- Nausea
- Weight loss
- Hyperpigmentation
- Salt craving
- Low blood pressure
It is essential to differentiate calcified adrenal glands with preserved function from those leading to adrenal insufficiency, which may require lifelong steroid replacement therapy.
Differential Diagnosis: When Calcification Isn’t Hemorrhage
Adrenal calcifications are not pathognomonic for prior hemorrhage. Other conditions can lead to adrenal gland calcification, and accurate differentiation is critical for appropriate management.
| Condition | Distinguishing Feature |
|---|---|
| Adrenal Tuberculosis | Often bilateral, associated with systemic TB |
| Histoplasmosis | Common in endemic areas, granulomatous infection |
| Adrenal Metastasis | May calcify post-treatment, usually asymmetrical |
| Pheochromocytoma | Can calcify, but usually has enhancing soft tissue mass |
| Congenital Adrenal Hyperplasia | May show calcification from repeated bleeding |
Management Strategies: Acute Hemorrhage and Long-Term Follow-Up
Management of adrenal hemorrhage depends on the phase and clinical presentation.
Acute Phase
- Stabilization: Manage blood pressure, fluid balance.
- Hormonal Support: Administer corticosteroids if adrenal insufficiency is suspected.
- Imaging Monitoring: Repeat CT/MRI to assess progression or resolution.
Chronic Phase and Calcification
- Observation: Asymptomatic, incidentally discovered calcifications require no immediate treatment.
- Endocrine Evaluation: Check adrenal function through serum cortisol, ACTH stimulation testing.
- Surgical Intervention: Rarely indicated unless associated with tumor or functional mass.
Practical Tips for Clinicians
- Always investigate bilateral adrenal calcifications, as they may indicate systemic illness or prior adrenal crisis.
- In neonates with adrenal calcification, follow-up imaging and endocrine assessment are recommended to ensure normal development.
- In adults, assess adrenal hormonal function even in asymptomatic patients with bilateral calcification.
- Consider infectious etiologies (TB, fungal infections) in patients with risk factors or relevant exposures.
- Avoid unnecessary adrenalectomy unless a functional or malignant lesion is suspected.
Future Directions in Research and Imaging
Emerging imaging techniques, such as dual-energy CT and high-resolution MRI, may help distinguish calcified hemorrhages from tumors with greater accuracy. Additionally, molecular testing and AI-enhanced imaging interpretation are being explored to improve early diagnosis and personalize treatment.
Researchers are also investigating the potential for adrenal tissue regeneration and stem cell therapies in the management of adrenal insufficiency—particularly relevant in cases of hemorrhagic destruction.
Conclusion: A Hidden Clue With Broad Implications
Adrenal hemorrhage calcification may appear to be a radiologic footnote, but it can hold vital clinical significance. From identifying prior hemorrhagic insults to flagging risks of adrenal insufficiency, calcification serves as a critical diagnostic clue. Through appropriate imaging, thorough clinical evaluation, and vigilant endocrine monitoring, clinicians can turn this often-overlooked finding into a cornerstone of personalized patient care.
Understanding the full spectrum of adrenal hemorrhage—from acute events to calcified sequelae—empowers healthcare providers to prevent complications, tailor treatments, and improve long-term outcomes in both pediatric and adult populations.
References
- Rao, R.H., Vagnucci, A.H., & Amico, J.A. (1989). Bilateral massive adrenal hemorrhage: early recognition and treatment. Annals of Internal Medicine, 110(3), 227–235. https://www.acpjournals.org/doi/10.7326/0003-4819-110-3-227
- Marti, J.L., Millet, J., Sosa, J.A., & Roman, S.A. (2012). Adrenal hemorrhage: evaluation of current imaging modalities. Journal of Surgical Research, 172(1), 111–116. https://www.journalofsurgicalresearch.com/article/S0022-4804(23)00504-8/pdf
- Simon, D.R., & Palese, M.A. (2009). Clinical update on the management of adrenal hemorrhage. Current Urology Reports, 10(1), 78–83. https://link.springer.com/article/10.1007/s11934-009-0014-y
- Vella, A., Nippoldt, T.B., & Morris, J.C. (2001). Adrenal hemorrhage: a 25-year experience at the Mayo Clinic. Mayo Clinic Proceedings, 76(2), 161–168. ttps://www.mayoclinicproceedings.org/article/S0025-6196(24)00046-6/fulltext
- Lonergan, G.J., et al. (2001). Pediatric adrenal masses: radiologic-pathologic correlation. Radiographics, 21(4), 995–1018. https://pubs.rsna.org/doi/10.1148/radiographics.21.4.g01jl15995
- Klose, M., et al. (2019). Adrenal insufficiency after bilateral adrenal hemorrhage. European Journal of Endocrinology, 181(5), 365–374. https://academic.oup.com/ejendo/article/190/5/G25/7663654



0 Comments