Lymph nodes may be small, but they play an outsized role in the immune system, acting as critical sentinels in the detection, response, and management of diseases. Among them, the lymph nodes located in the abdomen and pelvis are especially vital due to their proximity to key organ systems and their involvement in a wide range of medical conditions—from cancer and infections to autoimmune disorders. Despite their significance, these nodes often go unnoticed until disease manifests.
This article explores the function, structure, and clinical significance of abdominal and pelvic lymph nodes. We’ll discuss how they contribute to immune surveillance, detail the conditions that may affect them, and examine how modern diagnostic tools leverage their pathology for early detection and disease management. Understanding these nodes is not just an academic exercise—it can profoundly impact diagnostic accuracy and treatment strategies.
In This Article
Anatomy and Physiology of Abdominal and Pelvic Lymph Nodes
A Brief Overview of the Lymphatic System
The lymphatic system comprises a network of vessels, nodes, and organs responsible for fluid balance, immune surveillance, and fat absorption. Lymph nodes act as filters for harmful substances, housing lymphocytes that detect and destroy pathogens or abnormal cells. They are categorized by location, and in the case of abdominal and pelvic lymph nodes, they lie deep within the body cavity, connected by an intricate system of lymphatic vessels.
Key Lymph Node Groups in the Abdomen and Pelvis
The abdominal and pelvic lymph nodes are organized into various groups, typically named after nearby anatomical landmarks. Below is an overview:
| Lymph Node Group | Location | Drains Structures From |
|---|---|---|
| Celiac Nodes | Near the celiac trunk | Liver, stomach, spleen, pancreas, and upper duodenum |
| Mesenteric Nodes | Along the mesentery of the intestines | Small and large intestines |
| Para-aortic (Lumbar) Nodes | Adjacent to the aorta | Kidneys, adrenal glands, gonads, and posterior abdominal wall |
| Iliac Nodes (Common, External, Internal) | Along the iliac arteries and veins | Pelvic organs, perineum, gluteal region |
| Inguinal Nodes | In the groin area | Lower limbs, external genitalia, lower abdominal wall |
| Sacral Nodes | In front of the sacrum | Rectum and posterior pelvic wall |
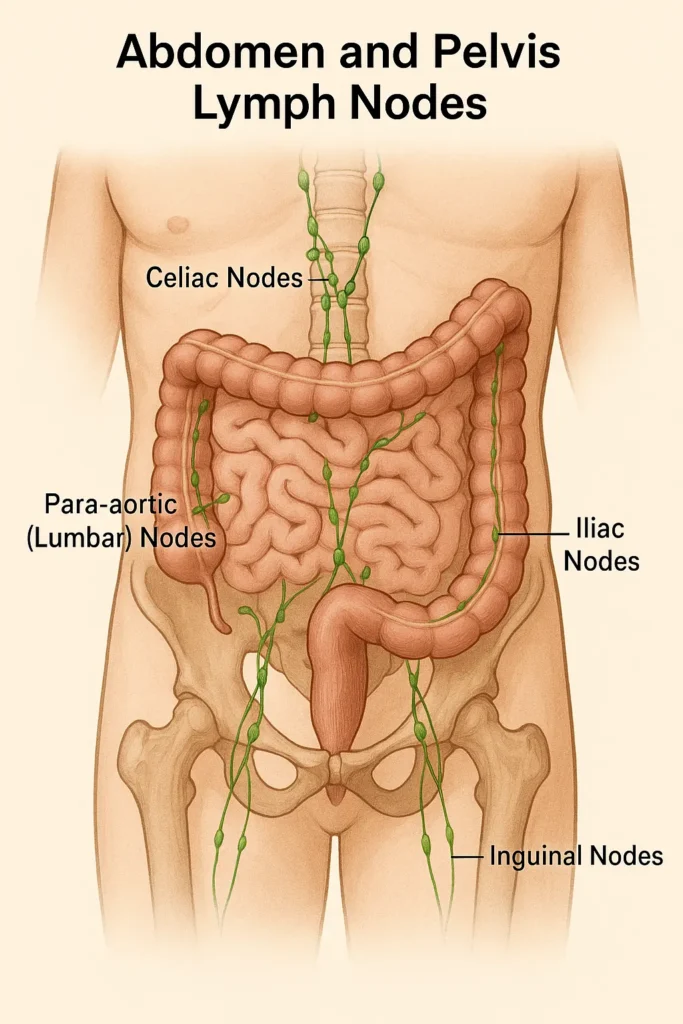
These lymph nodes receive lymphatic drainage from the gastrointestinal tract, reproductive organs, urinary system, and parts of the musculoskeletal system. Their role is essential not only in filtering lymph but also in immune system activation during infections or malignancies.
Functions of Abdominal and Pelvic Lymph Nodes
Abdominal and pelvic lymph nodes serve several key functions:
- Immune Surveillance and Response
These nodes are primary sites where antigen-presenting cells interact with lymphocytes. Upon recognizing a threat—such as bacteria, viruses, or mutated cells—they initiate an immune response, including the proliferation of T and B cells. - Filtration of Lymphatic Fluid
As lymph passes through these nodes, they trap pathogens, cellular debris, and potentially cancerous cells. This filtration is vital for preventing systemic spread of disease. - Sentinel Role in Cancer Spread
Because cancer cells often migrate via lymphatic pathways, abdominal and pelvic lymph nodes act as early indicators—or “sentinels”—of malignancy. Their enlargement or abnormal imaging appearance can be an early sign of metastatic spread.
Clinical Significance: Conditions Involving Abdominal and Pelvic Lymph Nodes
These lymph nodes are implicated in various conditions, ranging from benign inflammatory responses to life-threatening malignancies. Understanding their involvement can help clinicians make timely and accurate diagnoses.
1. Malignancies and Metastases
Abdominal and pelvic lymphadenopathy (enlargement of lymph nodes) is a hallmark feature in several types of cancer. Here’s how they relate to major cancers:
| Cancer Type | Common Lymph Node Involvement | Clinical Significance |
|---|---|---|
| Colorectal cancer | Mesenteric, para-aortic, iliac | Nodal involvement guides staging and prognosis |
| Cervical and ovarian cancer | Pelvic (iliac, obturator), para-aortic | Key for surgical staging and treatment planning |
| Prostate cancer | Pelvic and sacral nodes | Helps assess local vs. systemic spread |
| Testicular cancer | Retroperitoneal (para-aortic) nodes | First site of metastatic spread due to lymphatic drainage |
| Lymphoma (Hodgkin/Non-Hodgkin) | Widespread involvement | Diagnostic hallmark, used for staging and response assessment |
2. Infectious Diseases
Infectious causes of lymphadenopathy include:
- Tuberculosis (TB): Abdominal TB can cause caseating lymphadenitis, often diagnosed by imaging or biopsy.
- HIV: Generalized lymphadenopathy is a common feature.
- Yersinia and Salmonella: These can cause mesenteric lymphadenitis, often mistaken for appendicitis.
- Parasitic infections: Such as filariasis, which can lead to lymphatic obstruction and elephantiasis.
3. Inflammatory and Autoimmune Disorders
- Sarcoidosis: Often involves abdominal lymph nodes, particularly in multisystemic presentations.
- Systemic Lupus Erythematosus (SLE): Can cause reactive lymphadenopathy.
- Inflammatory Bowel Disease (IBD): Particularly Crohn’s disease, which may affect mesenteric nodes.
Diagnostic Tools for Abdominal and Pelvic Lymph Nodes
Timely identification of lymph node abnormalities is essential for early intervention. Several diagnostic modalities are used:
1. Imaging
- Ultrasound: Useful for superficial and pelvic nodes, particularly in gynecologic evaluations.
- CT (Computed Tomography): Gold standard for assessing node size, shape, and enhancement.
- MRI: Offers excellent soft-tissue resolution, often used in pelvic assessments.
- PET-CT (Positron Emission Tomography): Essential in oncological staging to detect metabolically active (cancerous) nodes.
2. Histopathological Examination
- Fine-Needle Aspiration (FNA): Minimally invasive, used to extract cells for cytology.
- Core Needle Biopsy: Provides tissue architecture, valuable in lymphoma diagnosis.
- Surgical Excision: Sometimes required for deep nodes when malignancy is suspected but cannot be diagnosed otherwise.
Interpreting Lymph Node Characteristics
| Feature | Benign Indication | Malignant Indication |
|---|---|---|
| Size | <1 cm (short axis) | >1.5 cm, especially if round |
| Shape | Oval with fatty hilum | Round, loss of fatty hilum |
| Margins | Well-defined | Irregular or spiculated |
| Internal Echo Pattern | Homogeneous | Heterogeneous, necrotic |
| Enhancement on Imaging | Mild or no enhancement | Strong, irregular, or ring-like enhancement |
Treatment and Management Strategies
Managing conditions involving abdominal and pelvic lymph nodes depends on the underlying disease.
For Cancer:
- Surgical Resection: Lymph node dissection is part of many oncologic surgeries for staging and therapeutic purposes.
- Radiation Therapy: Targeted radiation may be used when nodes are confirmed or suspected to harbor metastases.
- Systemic Therapies: Chemotherapy, immunotherapy, and targeted agents are often employed depending on histopathology and genetic profiling.
For Infections and Inflammation:
- Antibiotics/Antivirals: Tailored to the organism involved.
- Steroids/Immunosuppressants: Used in autoimmune conditions or sarcoidosis.
- Monitoring: Reactive nodes without alarming features may only require follow-up imaging.
When to Investigate Further: Red Flags in Lymphadenopathy
Not all enlarged nodes are dangerous. However, the following features warrant further investigation:
- Persistent enlargement (>4 weeks)
- Rapidly growing nodes
- Associated systemic symptoms (fever, weight loss, night sweats)
- Hard, immobile, or fixed nodes
- Abnormal lab findings (e.g., elevated LDH, abnormal blood counts)
These may point toward malignancy, tuberculosis, or other serious systemic illnesses.
Actionable Insights for Patients and Clinicians
- Early Detection Is Key: Many abdominal and pelvic cancers are silent until advanced stages. Vigilant attention to unexplained symptoms and appropriate imaging can catch disease earlier.
- Collaborative Care: Managing these conditions often requires input from gastroenterologists, oncologists, radiologists, and surgeons.
- Don’t Ignore the Nodes: When dealing with abdominal pain, gastrointestinal changes, or pelvic masses, always consider lymphatic involvement.
- Stay Informed: Patients with known risk factors—like family history of GI cancers, immunocompromised states, or chronic infections—should stay proactive with screenings.
Conclusion: A Silent System with Loud Implications
Abdominal and pelvic lymph nodes may not receive much attention in everyday discussions about health, but their clinical relevance is immense. They offer crucial insight into disease processes ranging from infections and autoimmune conditions to some of the deadliest forms of cancer. Understanding their anatomy, pathology, and diagnostic significance enhances our ability to detect disease early, treat it effectively, and improve outcomes. As diagnostic technologies advance and our understanding of the lymphatic system deepens, these small structures will continue to play a large role in the future of medicine.
References
- Gray, H. (2020). Gray’s Anatomy: The Anatomical Basis of Clinical Practice (42nd ed.). Elsevier.
- Cancer.Net Editorial Board. (2023). Lymph Node Metastasis. American Society of Clinical Oncology.
- World Health Organization. (2023). Tuberculosis. https://www.who.int/health-topics/tuberculosis
- National Comprehensive Cancer Network. (2024). Clinical Practice Guidelines in Oncology.
- Mayo Clinic Staff. (2023). Lymphadenopathy: Symptoms and causes. Mayo Clinic.
- Townsend, C. M., & Beauchamp, R. D. (2021). Sabiston Textbook of Surgery (21st ed.). Elsevier.
- Hricak, H. et al. (2022). Imaging the Pelvis and Abdomen: Current Concepts in Radiology. Radiology Journal.
- UpToDate. (2024). Approach to the adult with lymphadenopathy.
- NIH. (2023). The Human Lymphatic System. National Institute of Allergy and Infectious Diseases.
- Smith-Bindman, R., & Miglioretti, D. (2023). Radiation exposure from imaging tests in cancer evaluation. Journal of the American Medical Association.



0 Comments